How the Brain Heals and What Truly Drives Recovery
A Neurologist-Guided, Patient-Centered Roadmap
Stroke Recovery Is a Neurological Process — Not a Waiting Period
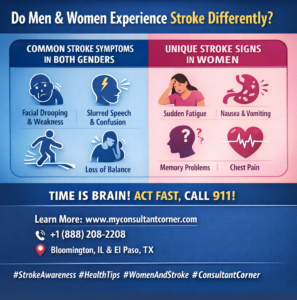
A stroke is not simply a sudden medical event; it is a neurological injury that disrupts the brain’s ability to control movement, speech, cognition, behavior, and vital bodily functions. Whether caused by an ischemic blockage or an intracerebral hemorrhage, stroke results in acute damage to brain tissue followed by a complex and evolving recovery process.
In the United States, nearly 800,000 people experience a stroke each year, making it one of the leading causes of long-term neurological disability. Advances in acute stroke treatment have significantly improved survival. However, survival is only the beginning. What follows is a prolonged and highly individualized process of neurological recovery.
For patients and families, this phase is often filled with uncertainty:
Will strength return? Will speech improve? How long does recovery take? Is rehabilitation truly effective?
From a neurological standpoint, recovery is best understood through two core principles:
- Stroke recovery is driven by brain plasticity, not time alone
- Rehabilitation is an active neurological treatment, not supportive care
Understanding these principles helps patients and caregivers move forward with clarity, realistic expectations, and hope.
How the Brain Heals After Stroke: Understanding Neuroplasticity
When a stroke occurs, part of the brain is injured or deprived of blood flow, leading to loss of neurons and disruption of neural networks. Importantly, this injury does not mean the brain is incapable of recovery. Instead, recovery depends on how surviving brain regions adapt over time — a process known as neuroplasticity.
What Is Neuroplasticity?
Neuroplasticity refers to the brain’s ability to reorganize, strengthen existing connections, and form new neural pathways in response to injury and experience. After a stroke, unaffected areas of the brain can partially assume functions previously handled by damaged regions. This biological adaptability is the foundation of rehabilitation.
Crucially, neuroplasticity is activity-dependent. The brain does not reorganize simply with rest or time. Recovery is driven by repetitive, meaningful, task-specific practice, which is why structured rehabilitation is so effective.
Early and Late Brain Recovery
In the first days to weeks after a stroke, the brain enters a period of heightened plasticity. Swelling subsides, inflammation decreases, and neural signaling stabilizes. During this phase, early improvements may reflect recovery of stunned but viable tissue.
While the most rapid gains often occur within the first 3–6 months, recovery does not stop there. Research shows that meaningful improvement can continue for 6–12 months and beyond, particularly when rehabilitation remains progressive and goal-directed.
Later recovery often involves:
- Refinement of motor control rather than large strength gains
- Improved balance, coordination, and endurance
- Gradual improvements in language and cognition
- Development of compensatory strategies that enhance independence
The idea that recovery “plateaus” early is often a reflection of reduced therapy intensity or lack of reassessment — not a true limit of neurological potential.
Rehabilitation Therapies That Drive Recovery
Stroke rehabilitation is not a single therapy or a one-size-fits-all program. It is a multidisciplinary neurological intervention designed to retrain the brain by engaging impaired neural networks repeatedly and purposefully.
Physical Therapy: Restoring Mobility and Balance
Physical therapy focuses on improving strength, coordination, balance, and gait. Weakness, spasticity, and impaired balance are common after a stroke and significantly affect independence.
Through task-oriented and repetitive movement training, physical therapy helps the brain re-map motor pathways, reduce fall risk, and improve functional mobility. Therapy evolves — from basic transfers to higher-level balance, endurance, and community mobility.
Occupational Therapy: Regaining Independence in Daily Life
Occupational therapy helps patients regain the ability to perform activities of daily living, such as dressing, bathing, eating, writing, and managing household tasks. Stroke often affects fine motor control, visual-spatial processing, and executive function — all critical for daily independence.
OT integrates motor, sensory, and cognitive systems, reinforcing purposeful use of affected limbs and promoting functional recovery rather than learned non-use.
Speech and Language Therapy: Communication and Swallowing
Stroke can affect language (aphasia), speech clarity (dysarthria), cognition, and swallowing (dysphagia). Speech-language therapy addresses:
- Language comprehension and expression
- Speech articulation and voice control
- Cognitive-communication skills
- Swallowing safety and nutrition
Recovery in this domain may be gradual, but meaningful gains can continue long after motor recovery stabilizes. Early swallowing evaluation is essential to reduce aspiration risk and medical complications.
Cognitive Rehabilitation: Attention, Memory, and Executive Function
Cognitive changes after stroke are common and frequently underrecognized. Patients may struggle with attention, memory, processing speed, or executive skills — even when physical recovery appears strong.
Cognitive rehabilitation helps patients develop new strategies to strengthen preserved neural pathways and compensate for deficits. Recovery in this domain often continues later into the recovery process, reinforcing the importance of ongoing reassessment.
Early Recovery: The First Weeks Matter — But Don’t Define Everything
The first days to weeks after a stroke represent a critical window of opportunity. During this phase, early mobilization and rehabilitation — when medically appropriate — improve functional outcomes and reduce complications.
That said, early appearance does not define long-term outcome. Neurologists caution against premature prognostication. Patients may appear severely impaired early on yet make meaningful gains over time, while others with milder strokes may struggle due to secondary complications.
Common early challenges include:
- Fatigue
- Fluctuating weakness or tone
- Speech or swallowing difficulty
- Cognitive slowing or confusion
- Emotional distress
These challenges are common and treatable. Addressing them early improves participation in rehabilitation and long-term outcomes.
What Really Predicts Stroke Recovery
Recovery is shaped by multiple interacting factors — not a single variable.
What Matters Most:
- Quality, timing, and intensity of rehabilitation
- Patient engagement and education
- Ongoing neurological oversight
- Social and caregiver support
- Management of medical and neurological complications
What Matters Less Than Commonly Believed:
- Age alone (older adults retain neuroplastic capacity)
- Early severity as a fixed predictor
- Arbitrary recovery timelines
From a neurologist’s perspective, trajectory over time is far more meaningful than a single snapshot.
Cognitive, Emotional, and Behavioral Recovery
Physical recovery is often the most visible aspect of stroke rehabilitation, but cognitive and emotional changes can be equally impactful.
Cognitive Changes
Difficulties with attention, memory, executive function, or visual-spatial processing may affect independence, work, and social engagement. These deficits may emerge gradually and improve over months to years.
Emotional and Mood Changes
Depression, anxiety, irritability, emotional lability, and apathy are common after stroke. These symptoms reflect biological changes in mood-regulating brain networks combined with the emotional stress of recovery. They are not personal failures — and they are treatable.
Behavioral Changes
Some patients experience changes in behavior or personality, particularly after frontal or subcortical strokes. Education and support help families understand that these changes are neurological in origin.
Addressing cognitive and emotional recovery improves quality of life, rehabilitation participation, and long-term outcomes.
Preventing Complications and Secondary Stroke
Recovery must occur alongside secondary stroke prevention. Stroke survivors face an increased risk of recurrence, particularly in the first year.
Key elements include:
- Control of blood pressure, diabetes, and cholesterol
- Management of atrial fibrillation or other cardiac conditions
- Medication adherence (antiplatelets, anticoagulants, statins)
- Fall prevention and safety strategies
- Treatment of spasticity, pain, seizures, fatigue, and sleep disorders
Neurologists help tailor prevention strategies to the stroke mechanism and individual risk, ensuring protection of recovery gains.
Long-Term Recovery: Months to Years After Stroke
Recovery does not end when formal therapy becomes less frequent. Long-term recovery often involves refinement rather than dramatic change, including better coordination, endurance, language fluency, and confidence.
The concept of a “plateau” is often misleading. Reassessment frequently reveals opportunities for renewed therapy, adaptive strategies, or technology-assisted rehabilitation.
Long-term goals may include:
- Returning to work or hobbies
- Driving evaluation
- Managing fatigue
- Enhancing independence and safety
Neurological follow-up ensures recovery plans evolve alongside life goals.
Caregivers, Technology, and the Future of Recovery
Caregivers play a central role in reinforcing therapy, ensuring safety, and supporting emotional adjustment. Education reduces burnout and improves outcomes for both patients and families.
Technology and tele-rehabilitation are increasingly important, especially for patients with mobility or access limitations. Virtual therapy, wearable monitoring, and tele-neurology support continuity of care and long-term engagement.
The future of stroke recovery lies in personalized, neurologist-guided rehabilitation enhanced by thoughtful use of technology.
How Consultant Corner Supports Post-Stroke Recovery
Stroke recovery is a longitudinal neurological journey, not a single episode of care. Consultant Corner provides neurologist-led, evidence-based guidance throughout every phase of recovery.
We support patients and families by:
- Interpreting recovery trajectories
- Adjusting rehabilitation strategies
- Managing late-emerging complications
- Coordinating care across disciplines
- Providing accessible virtual neurology follow-up
Our goal is to help patients continue making meaningful gains — with clarity, confidence, and expert neurological support.
Contact Consultant Corner
📞 Phone: +1 (888) 208-2208
📧 Email: info@myconsultantcorner.com
🌐 Website: www.myconsultantcorner.com
Consultant Corner — Thoughtful, Evidence-Based Neurology Care for Recovery and Beyond.